Safety is Our Top Priority
healthsurge cares about the well-being of our healthcare professionals and We want to do our part to help fight against the global pandemic.
Need Statement
SARS-CoV-2 is a novel coronavirus that has become a pandemic. Current data suggests that the virus is spread primarily through contact with an infected person’s respiratory droplets (i.e., from coughs or sneezes). As of May 2020, it has infected over 4 million people worldwide (cdc.gov). Unfortunately, healthcare providers in areas that have been deeply affected by the virus do not have the necessary personal protective equipment (PPE) to safely care for patients. Most notably, the lack of face masks and face shields has been a significant issue. Under the guidance of Natalie Trinh, Dr. Aditi Sharma, and Justin Huang, the members of HealthSurge split into two teams to contribute an easily manufacturable non-powered mask to frontline workers.

Filter Media – Frances, Mark, and Raymond
Through our team’s research on novel filter media, we focused on both mechanical and electrostatic filtration methods. Mechanical filtration depends on the physical arrangement of fibers through diffusion, interception, and inertial impaction (Figure 1). Electrostatic filtration depends on chemical properties of the fibers attracting target particles. After researching novel filter materials discussed in peer-reviewed papers, we decided to focus our efforts on electrospun nanofibers because of success in performing both mechanical and electrostatic filtration methods on air-borne particles.

Figure 1. The four primary filtration mechanisms.
Electrospun nanofibers are fibers created through electric force (Figure 2) and are typically resins or carbon based polymers. They can be spun to create random patterns and can be scaffolded with a supporting polymer to increase mechanical integrity. These are great at filtering because the nanofiber mats produced can have very small pores and have other materials integrated to increase filtration efficiency. This material met all of our criteria but still needed to go through initial testing.
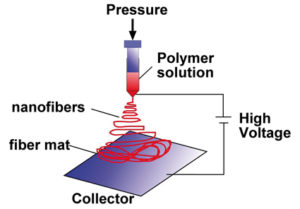
Figure 2. Electrospinning Setup
We used this material as a basis for research into existing materials on the market that are similar or made in a similar process. We investigated patents for current filters sold by commercial air filtration manufacturers with the goal of identifying materials that can be repurposed to meet the demand for filter media for respirators. We found a few options, sent them for testing, and are still awaiting results. For now, we continue to investigate the possibility of repurposing HEPA filters, perhaps designing mechanisms to ensure their integrity to avoid the inhalation of fiberglass particles and other options.
Respirator – Jessica, Jeremy, and Juliana
Our first task was to design a mechanism to determine the amount of filter surface area needed for comfortable airflow (Figure 3). Solidworks designs were generated by our team which were then 3D printed and tested by mentor Justin Huang. It was determined that approximately 500 sq centimeters of filter media surface area are necessary for users to breathe without restricted air flow.
 Figure 3. Solidworks Assembly of the sliding mechanism
Figure 3. Solidworks Assembly of the sliding mechanism
From here, the team started designing a vacuum formable filter cartridge in Solidworks that was compatible with standard 3M respirators. Our goal is to continue refining our designs before sending them off to be manufactured and donated to healthcare providers.
Sterilization
Seven methods of resterilization were researched for standard surgical and N-95 masks while we were prototyping respirator designs and identifying filter materials. These methods of sterilization were Plasma Hydrogen Peroxide (STERRAD), Autoclave (Steris), Vapor Hydrogen Peroxide, Moist Heat, Ultraviolet Germicidal Irradiation (UVGI), NO2 Sterilization, and Ozone Sterilization (low temperature). Based on our research, Vapor Hydrogen Peroxide was deemed the best option for resterilizing used masks at this time, followed by UVGI. This conclusion was based on:
1) the resources/machinery hospitals already have access to or own
2) the amount of time needed to sterilize the mask
3) efficacy of the sterilization cycle
4) the amount of damage to the mask after sterilization